The Difference Between Bacterial Colonization and Infection: A Focus on Dental Health
Understanding the difference between bacterial colonization and infection is crucial for appreciating the dynamics of our body's interaction with microbes, particularly in the context of oral health. Bacterial colonization refers to the presence of bacteria on a surface without causing disease or harm. These bacteria exist in a balanced relationship with their host, contributing to various physiological processes. Infection, on the other hand, occurs when bacteria invade tissues, multiply, and trigger an immune response, leading to symptoms of illness.
Bacterial Colonization vs. Infection
Bacteria are found everywhere in and on the human body, with trillions of microbes coexisting in a complex ecosystem. Colonization is a natural and often beneficial process where bacteria inhabit specific areas in the body without causing harm. For example, the gut microbiome plays a crucial role in digestion and immune function, while skin bacteria provide protection against harmful invaders.
On the other hand, an infection occurs when harmful bacteria breach the body's defenses, multiply uncontrollably, and trigger an inflammatory response. This response can lead to symptoms such as fever, pain, swelling, and tissue damage. Infections require intervention, such as antibiotics or other treatments, to restore health.
Dental Plaque: A Case of Normal Colonization
Dental plaque is a biofilm that naturally forms on teeth. It is made up of a variety of bacteria, saliva proteins, and food particles. Contrary to popular belief, plaque itself is not inherently harmful. In fact, for most of human history, plaque did not cause significant dental issues like cavities or gum disease.
Throughout the Paleolithic era, humans maintained relatively good dental health despite the presence of plaque. Their diets consisted mainly of unprocessed foods such as meat, vegetables, fruits, and nuts, which did not provide the same substances for harmful bacterial activity as modern diets do. As a result, tooth decay and gum disease were rare, even though plaque was present.
The Onset of Dental Problems with Farming
The introduction of agriculture brought about a significant change in human diets as people started consuming more carbohydrates, especially grains. This shift led to new challenges for oral health, particularly due to the easy fermentation of carbohydrates by oral bacteria, especially in processed foods.
When carbohydrates are eaten, oral bacteria, such as Streptococcus mutans, ferment these sugars and produce lactic acid. This acid lowers the pH in the mouth, creating an acidic environment that can weaken tooth enamel. Over time, repeated acid attacks can lead to the formation of cavities.
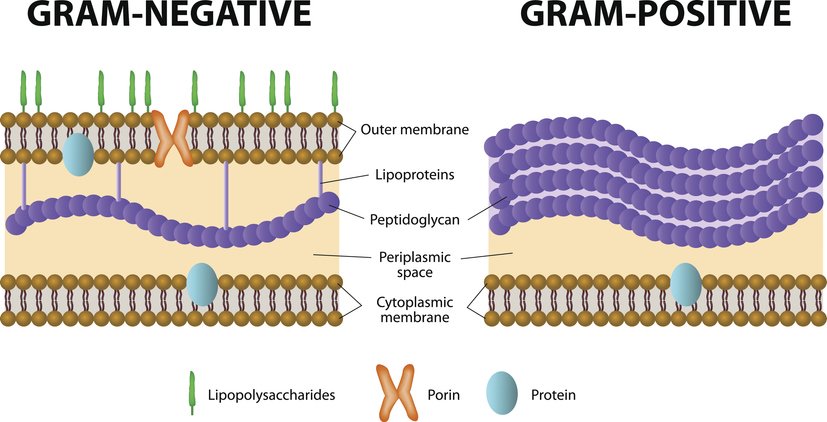
Furthermore, the adoption of a carbohydrate-rich diet created an optimal environment for the growth of gram-negative anaerobes like Porphyromonas gingivalis, a bacterium linked to periodontitis. These bacteria thrive in low-oxygen environments and produce lipopolysaccharides (LPS) or endotoxins. LPS triggers a significant inflammatory response in the gums, leading to tissue destruction and the advancement of gum disease.
The Role of Fermentation and pH in Tooth Decay
Oral bacteria ferment carbohydrates, which is a critical factor in tooth decay. When sugars and starches from foods like bread, pretzels, crackers, and chips are broken down by bacteria, the resulting acid lowers the mouth's pH. A healthy mouth typically has a pH of around 7 (neutral), but after consuming carbohydrates, the pH can drop below 5.5, which is the threshold at which enamel begins to demineralize.
As the enamel erodes, cavities form, providing more surfaces for bacteria to colonize and further exacerbate the problem. This cycle of carbohydrate consumption, acid production, and enamel erosion is at the heart of most dental decay issues in modern populations.
Gram-negative Anaerobes and Periodontitis
Porphyromonas gingivalis and other gram-negative anaerobes are particularly problematic because they do more than contribute to decay; they actively cause periodontal disease. These bacteria release endotoxins that trigger inflammation in the gum tissues. Chronic inflammation leads to the destruction of the tissues supporting the teeth, including the alveolar bone, eventually leading to tooth loss if left untreated.
Periodontitis is a severe condition that not only affects the gums and teeth but is also linked to systemic health issues, including cardiovascular disease, diabetes, and even Alzheimer's disease, due to the inflammatory burden it places on the body.
Xylitol: A Modern Solution with Caveats
Xylitol, a sugar alcohol used as a sweetener, has gained popularity for its purported dental benefits. It is known to reduce the levels of harmful bacteria in the mouth, particularly Streptococcus mutans. Xylitol interferes with the bacteria's ability to metabolize sugar and produce acid, thus reducing the risk of cavities.
While xylitol can diminish plaque colonies, it's essential to recognize that it does not address the root cause of most dental problems—processed carbohydrates. Xylitol might reduce bacterial activity, but as long as diets remain high in processed carbohydrates like bread, pretzels, and crackers, the risk of dental decay and gum disease remains high.
Conclusion
The history of human oral health provides valuable insights into the impact of diet on our teeth and gums. In the Paleolithic era, when diets were free from processed carbohydrates and refined sugars, plaque was a normal part of oral health and did not lead to widespread dental problems. However, with the advent of agriculture and the introduction of carbohydrate-rich foods, the incidence of tooth decay and gum disease skyrocketed.
The fermentation of sugars by oral bacteria, leading to acid production and a drop in pH, is a significant factor in the development of cavities. Additionally, the proliferation of gram-negative anaerobes like Porphyromonas gingivalis in response to these dietary changes has led to an increase in periodontal disease.
While modern solutions like xylitol can help reduce the impact of harmful bacteria, the most effective way to protect oral health is to reduce the consumption of processed carbohydrates and avoid foods high in linoleic acid from seed oils. A whole-food diet that includes animal-based foods with their natural fats and is devoid of processed carbohydrates and vegetable oils is the best strategy for maintaining both oral and overall health.